Originally published in ACRP’s Clinical Researcher on June 20, 2023
Thanks to social media platforms and their ability to widely disseminate information, whether fact or fiction, we live in a society where words and terms “go viral” almost as fast as video clips do. We are often inundated with terms like “diversity,” “equity,” “inclusion,” and “social determinants of health.” These particular words and terms are more than just descriptors though—they are necessary to acknowledge and accept in order to progressively move our field forward. Harvard is even offering a class on the subject!
Mission-driven companies that offer eClinical and digital healthcare solutions know that using technological advancements in order to provide access to more patients—effectively closing the inequality gap—is necessary for the betterment of the clinical research field at large.
The U.S. Department of Health and Human Services (HHS) states that the “social determinants of health (SDOH) are the conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks.”
According to HHS information tied to its Healthy People 2030 initiative, SDOH can be grouped into five categories:
- Economic Stability
- Education Access and Quality
- Healthcare Access and Quality
- Neighborhood and Built Environment
- Social and Community Context
Basically, SDOH are social and economic factors that influence the health and well-being of individuals and their local communities. These factors are shaped by the distribution of money, power, and resources—impacting a patient’s access to quality healthcare and therefore having a significant impact on their health outcomes.
The World Health Organization (WHO) defines “social determinants of health equity” similarly as “the conditions in which people are born, grow, live, work, and age.” These conditions, again, include factors such as education, employment, housing, access to healthy food, transportation, exposure to stressors and violence, and access to healthcare and social support networks. SDOH are also influenced by broader social factors such as racism, discrimination, and poverty—hence the addition of the word “equity.”

The Many Pain Points of SDOH
The impact of SDOH on a single patient’s health and healthcare access is significant. For example, research has shown that people who live in poverty are more likely to experience more serious health outcomes such as chronic diseases, mental health disorders, and premature death. Similarly, people who experience discrimination based on their race, ethnicity, or gender are more likely to experience negative health outcomes. For example:
- People with lower incomes have a higher risk of chronic diseases such as diabetes and heart disease.
- Individuals who live in neighborhoods with limited access to healthy food (e.g., “food deserts”) are more likely to have poor nutrition and suffer from obesity.
- Lack of access to quality education can result in reduced economic opportunities and contribute to poor health outcomes.
- Unhoused citizens face significant health challenges, including chronic diseases, mental illness, and substance abuse.
- Racism and discrimination can lead to poor health outcomes for marginalized groups, including higher rates of chronic disease and metal health disorders.
SDOH also have adverse influence on the utilization and costs of care. People who experience social and economic disadvantages are more likely to have severely limited access to healthcare services, which can lead to delayed diagnoses, untreated illnesses, and increased healthcare costs over time (see: Health Equity Tracker). Therefore, SDOH can also have a significant impact on the design, implementation, and outcomes of clinical studies; for example, through their influences on these mechanisms:
- Recruitment: SDOH can affect efforts to recruit study participants, as individuals from low-income households and/or limited education may be less likely to participate in clinical trials due to transportation or time constraints; mistrust of doctors and other healthcare professionals; or a lack of awareness of their eligibility.
- Retention: Participants from marginalized or underrepresented populations may face social and economic barriers that make it challenging to complete clinical trials, such as competing responsibilities or lack of social support networks.
- Data collection: SDOH can impact the quality and completeness of data collected during clinical research. For example, a patient’s socioeconomic status may affect his or her ability to provide accurate medical history or access to healthcare resources that could affect the interpretation of clinical outcomes.
- Intervention effectiveness: SDOH can impact the effectiveness of interventions evaluated in clinical research. For example, social and economic factors such as housing conditions, access to healthy food, and social support networks can impact and individual’s ability to adhere to treatment or achieve positive health outcomes.
Putting eClinical on the Case
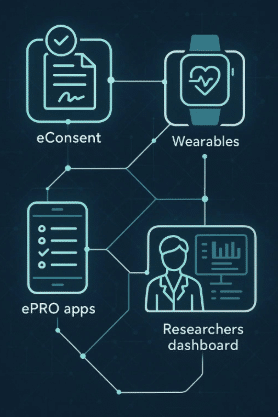
Considering all of the factors listed above, it is crucial for clinical study teams to address the realities of SDOH when designing and conducting trials. This can include integrating eClinical technology platforms and solutions to assist in executing strategies to recruit and retain diverse study populations, passively collecting patient data, and incorporating interventions (such as “nudging” patients to complete their eDiaries) to ensure patient compliance.
Digital healthcare providers can help address SDOH by leveraging the technology solutions they create to applaud and support the strides regulatory bodies and international governmental agencies are making to bring equitable, quality access to healthcare and clinical trials worldwide. Additionally, we must also work to provide the solutions to these complex challenges ourselves. Here are some ways digital healthcare platforms can help:
- Telemedicine can provide patients in remote or underserved areas with access to quality healthcare providers of their choice.
- Digital health and eClinical study apps and wearable devices can help patients manage chronic conditions such as diabetes and hypertension.
- Virtual healthcare platforms can improve mental health access for individuals in need of behavioral healthcare services.
- Health information technology can improve care coordination and help healthcare providers better manage patient care.
- Digital tools can be used to promote health education and awareness, such as healthy eating and physical activity.
Further, eClinical solutions can support virtual, hybrid, and decentralized clinical trials worldwide. Remote patient monitoring via wearables, biosensors, other medical devices, telehealth visits, and communications via SMS or other messaging apps remove barriers such as costs to travel to a site and a clinical trial being inaccessible due to geographical locations.
The Big Picture
Virtual clinical trials and digital healthcare are the future of real-world solutions for many of the woes facing the clinical research enterprise. Technology platforms help to close the gap in equity and bring quality healthcare and equal opportunities to participate in clinical trials—saving patient lives.
In addition to helping patients feel empowered to take charge of their own health, digital and wearable technology solutions benefit the clinical research industry and healthcare overall. Improving the gathering of quality data and increasing diversity within the patient participant population will lead to more accurate and representative data within clinical studies—eventually impacting drug therapies, treatment protocols, and healthcare at large.
To reiterate, SDOH play a significant role in health outcomes. They are an important and often overlooked aspect of a patient’s health and well-being. Acknowledging these challenges and barriers to fair and equitable access to quality healthcare, and therefore the potential recruitment into a clinical trial, is just the first step. Understanding and addressing these factors are crucial for improving patient-reported outcomes and reducing the operational costs to successfully complete a clinical study.
It is imperative that eClinical solutions and digital healthcare providers work together to close the equity gap. This is not only beneficial to all patients around the world, but it is constructive for the clinical research enterprise as well. Reaching out to and recruiting more diverse and underrepresented patient populations to participate in clinical trials is valuable in that leads to diversified, real-world data and therefore real-world evidence about how, for example, a chronic disease might present itself differently in various populations. Analyzing wide-ranging data leads to learning more about our patients around the world—how different treatment plans and drug therapies can be applied to distinct patient profiles, hopefully leading to improved treatments and therapies for a healthier global population.
Conclusion
Aside from the benefits to general healthcare and to our specific field of clinical research, focusing on SDOH is simply the right thing to do. By focusing on these challenges and using innovative technology platforms and wearable devices to address them, we can create a more equitable and just healthcare system, with better access to clinical trials, that promotes health for all patients—worldwide.