The rise of wearable sensors is reshaping the way healthcare professionals collect and interpret patient data. By enabling continuous, real-time monitoring outside clinical environments, these devices are improving treatment personalization, adherence, and early intervention. For clinical innovators, wearable sensor technology represents a key step toward scalable, data-driven healthcare delivery.
Remote patient monitoring (RPM) powered by wearable sensors has moved from a niche technology to a foundational part of decentralized and hybrid clinical models. Understanding their role, functionality, and potential is essential for future-ready healthcare systems.
Understanding Wearable Sensors in Healthcare
Wearable sensors are compact, non-invasive devices designed to measure physiological parameters such as heart rate, oxygen saturation, body temperature, and activity levels. They transmit this data digitally for continuous analysis and clinical decision-making.
Core Functionality
These sensors use biosensor technology to detect changes in biological signals and convert them into digital information that can be processed by healthcare platforms or monitoring systems.
Integration with Digital Health Ecosystems
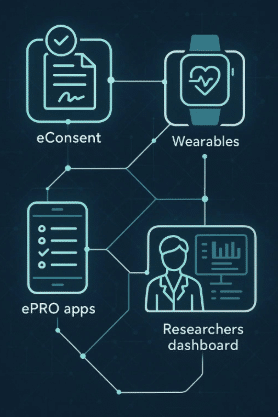
Modern wearable sensors seamlessly integrate into broader clinical data infrastructures, including decentralized clinical trial (DCT) platforms and remote care ecosystems, ensuring secure and consistent data flow.
The Role of Biosensor Technology
At the heart of wearable innovation lies biosensor technology. This technology allows for the precise detection and interpretation of biological processes in real-time.
Types of Biosensors Used
Common examples include electrochemical, optical, and piezoelectric sensors. Each is designed to capture specific physiological markers relevant to different therapeutic areas.
From Data Capture to Clinical Insights
The raw data from biosensors is processed using advanced analytics to generate actionable insights for clinicians, researchers, and sponsors. This supports early detection, continuous assessment, and data-driven decision-making.
Enabling Digital Endpoints in Clinical Trials
Wearable sensors are key enablers of digital endpoints, which allow for continuous, objective measurement of patient outcomes.
Continuous and Passive Monitoring
Unlike traditional episodic check-ins, wearables gather health data around the clock. This provides a more comprehensive picture of a patient’s condition and response to treatment.
Improving Endpoint Precision
Digital endpoints derived from wearable data minimize human error and subjectivity, increasing the reliability of clinical findings.
Regulatory Acceptance
Regulatory agencies are increasingly recognizing digital endpoints as valid tools for efficacy and safety evaluation, expanding their role in modern clinical trials.
Enhancing Patient Adherence and Engagement
Patient adherence remains a critical factor in both clinical trials and chronic disease management. Wearable sensors can make participation and ongoing monitoring more manageable.
Passive Data Collection
Because sensors function automatically, participants are not burdened by frequent manual entries, leading to higher adherence rates.
Real-Time Feedback
Devices often provide users with immediate feedback on their activity levels or vital signs, reinforcing healthy behavior and engagement.
Personalized Support
Data collected through sensors can be used to create personalized interventions, improving both adherence and outcomes.
Driving Innovation in Remote Patient Monitoring (RPM)
Remote patient monitoring extends the reach of healthcare beyond the clinic. Wearable sensors are the backbone of this model, providing reliable and continuous patient data.
Expanding Access to Care
Wearables enable healthcare providers to track patients in rural or underserved regions, reducing the need for in-person visits.
Early Detection and Intervention
Continuous monitoring allows clinicians to detect anomalies early, often before symptoms become severe, improving the chances of timely intervention.
Reducing Hospital Readmissions
With improved tracking and proactive care, wearable-driven RPM helps minimize unplanned hospital visits and readmissions.
Integration with Decentralized Clinical Trial (DCT) Technology
Decentralized clinical trials rely heavily on wearable sensors for accurate, real-world data collection.
Seamless Data Capture
Sensors transmit data directly to DCT tech stacks, ensuring real-time visibility for research teams.
Lower Participant Burden
By reducing travel requirements and on-site assessments, wearables make decentralized participation more practical and inclusive.
Improving Trial Efficiency
Continuous monitoring provides cleaner datasets, reduces protocol deviations, and accelerates timelines.
Data Management and Security in Wearable Monitoring
As data volume grows, secure handling and analysis of wearable data are critical.
Interoperability with Clinical Systems
Data from multiple devices must integrate smoothly into existing electronic data capture (EDC) and clinical trial management systems (CTMS).
Encryption and Privacy Protection
Wearable data is encrypted during transmission and storage to protect participant confidentiality and comply with data privacy regulations.
Data Validation and Quality Control
Automated systems ensure accuracy and integrity, preventing inconsistencies in large-scale remote monitoring projects.
Applications Across Therapeutic Areas
Wearable sensors are being applied across diverse medical and research fields.
Cardiology
Devices tracking ECG and heart rate variability provide continuous cardiac insights, supporting early detection of arrhythmias.
Diabetes Management
Continuous glucose monitors (CGMs) allow real-time tracking of blood glucose levels and lifestyle-related variations.
Oncology and Neurology
Activity tracking and physiological monitoring help evaluate fatigue, pain, and sleep—important indicators in cancer and neurodegenerative studies.
Emerging Trends in Wearable Sensor Technology
Innovation in wearable design continues to advance usability and accuracy.
Miniaturization and Comfort
Modern wearables are smaller, lighter, and more discreet, enhancing patient comfort and compliance.
Multi-Sensor Integration
Future devices will combine multiple biosensors into a single platform, allowing for comprehensive physiological monitoring.
AI-Powered Insights
Machine learning models are being developed to interpret sensor data and predict health outcomes with greater precision.
Conclusion
Wearable sensors are transforming remote patient monitoring by bridging the gap between continuous data collection and clinical decision-making. Through biosensor innovation, digital endpoints, and DCT integration, these devices empower clinicians to monitor patients more effectively and improve outcomes.
For clinical innovators, wearable sensors represent more than just technology they are a gateway to more inclusive, efficient, and data-rich healthcare systems. As the field evolves, their role in shaping the future of patient monitoring and decentralized research will only continue to expand.
FAQs
What are wearable sensors used for in healthcare?
They are used to continuously monitor vital signs and physiological parameters to support remote care and clinical research.
How do wearable sensors improve remote patient monitoring?
They enable real-time tracking and analysis, allowing early detection of health issues and reducing the need for frequent clinic visits.
Are wearable sensors accurate enough for clinical use?
Modern biosensor technology has significantly improved accuracy, making these devices reliable for regulated healthcare applications.
What role do wearable sensors play in decentralized trials?
They allow remote data collection and real-world evidence gathering, enhancing trial efficiency and patient participation.
How is wearable sensor data kept secure?
All transmitted data is encrypted and stored according to healthcare data privacy regulations to ensure patient confidentiality.